Progress in medical science can be painful. It’s no joke. Technology such as PACS and digital imaging can cause repetitive strain injuries for radiologists. And that’s just the beginning.
Radiology workstations designed ergonomically can help decrease the frequency and severity of repetitive strain injury. Use of ergonomic principles can vary from simple changes to equipment that changes the way radiologists work and eliminates the cause of many injuries.
You’ve heard the term for several years now. But what exactly is an ergonomic workstation, and how does it make things better?
Let’s start with the basics.
What is an ergonomic approach?
Almost every activity involved in a radiologist’s job can lead to some type of repetitive injury.
As a radiologist today, your job includes:
- Viewing high contrast images in a dark environment multiple hours per day
- Utilizing speech mics with Speech recognition software
- In certain cases, performing procedures
- Reporting test results
- Preparation of lectures and presentations
- More commonly, these tasks are being performed at home or from teleradiology workstations.
This is just a brief list of activities performed requiring repetitive motions.
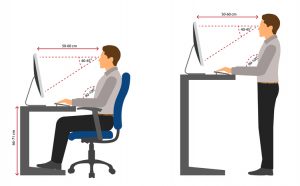
Ergonomic workstations are designed to minimize the need for and impact of repetitive motions such as standing, bending, twisting, and leaning in performing your job. Once these stressors are minimized, you can be more comfortable and productive when working.
What does an ergonomic workstation look like?
Ergonomic equipment for workstations varies by profession. As it relates to radiology workstations, ergonomic equipment includes:
- Desks/tables that have:
- Sit to stand adjustment capability
- Ability to change monitor height independent of worksurface
- Ability to easily and quickly change focal depth of monitors
- Large usable worksurface to provide space for radiologist’s equipment: multiple keyboards and mice, voice recognition mic, trackball, etc. . . Ideally a single surface to maximize useable space in a given footprint
- Ability to be quickly and easily adjusted/set up for each radiologist using the station
- Dimmable back lighting to reduce eye strain
- Electric sit to stand workstations/desks
- Monitors that:
- Meet ACR and FDA standards for brightness and resolution, ensuring images are DICOM Calibrated for proper diagnosis
- Include productivity tools with the ability to dim worklist panels, limiting ambient light causing eye strain. Cursor wrap functions eliminating continuous scrolling over the worksurface
- Maximize viewing clarity from various angles
- Reduce stress by offering adjustable height and angle
- Chairs that provide
- Vertebral support
- Head support
What should you consider before implementing an ergonomic approach at your radiology practice?
Implementing an ergonomic approach is more than buying equipment that has a list of features. It is important to see how specific features impact your patient care, medical staff, and overall satisfaction of the team.
A comprehensive ergonomic workflow rollout address every aspect of the practice and includes proper training on the use of the equipment as well as how can prevent injuries.
Technicians in radiology can benefit from an ergonomic approach as well. Important areas to consider for these team members includes:
- Manipulation of equipment necessary for performing procedures
- Transportation of the equipment
- Sit/stand desks for MRI and CT technicians
- Positioning of patients for completion of the procedure
- Ergonomic seating
How Does an Ergonomic Workstation Help Your Practice?
Ergonomics offers more than physical benefits. It results in increased productivity and efficiency, increased accuracy of reporting, a comfortable work environment, improved employee retention, and improved patient care.
The Association for Talent Development1 indicated that there are several factors that are improved when you focus on health and wellness:
- absenteeism
- retention and turnover
- productivity
- employee engagement
The costs associated with these factors is not small.
When an employee is injured, employers pay for more than the worker’s medical treatment. In its “NSC Injury Facts 2017,” the National Safety Council (NSC) calculates the average cost of an injury at $31,0002.
Radiation therapists appear to be at considerable risk for work-related musculoskeletal injuries, which corresponds with findings of studies on health care employees. They are reported to have a high prevalence of injuries (76%)3. In fact, 58% of radiologists report symptoms of repetitive stress injury (many spend over 8 hours per day at their desks).
The most common site-specific injury is the lumbar back, followed by the neck and shoulders3. Other injuries can include repetitive stress injuries, visual problems, and headaches.
Productivity and Efficiency
When an ergonomic approach is used, staff can avoid bending, twisting, and awkward positions that cause fatigue, soreness, and lost time, as well as decreased comfort as the workday progresses.
Employees can be happier and have more energy when they can be comfortable when they work. It’s easy to see that more energy put into helping patients results in patients who are happier with the care they receive.
Accurate Data Entry: A Surprising Benefit
Initially you might not consider that an ergonomic approach to Radiology workstations could impact the accuracy of data entry. However, consider that you would have a higher level of fatigue throughout the day when you have a high level of stress on your body. Errors are more likely due to the higher level of stress and fatigue that results in decreased focus.
Ergonomic equipment increases safety and comfort throughout the day, meaning that employees are safer, more comfortable, and less fatigued.
A Comfortable Radiology Workstation adds Value and Savings
When care providers can adjust table height, view records through an optimally sized and correctly positioned monitor, and move easily around the facility/unit, they are more comfortable and experience less fatigue. This means that strain on backs, wrists, and necks is drastically reduced, or eliminated. Ergonomic workstations designed to the unique demands of a job helps the radiology team do their job effectively and efficiently in comfort.
A ROI Comes in Many Forms
By now you realize that implementing an ergonomic approach requires investment of time and money.
Considering the costs of worker’s compensation, rehabilitation, and training of new radiologists, it is easy to see how you can quickly realize a return on your investment.
The biggest savings are seen in:
- Less time off for injury
- Fewer staff injuries and worker’s compensation claims
- Greater accuracy in reporting and patient care
- Healthier and happier staff with less turnover
When preventable injuries, burnout, and staff error are avoided, money typically spent on these items can now be spent where it is needed most.
Improved Patient Care is the Ultimate Reward
Imagine the improved patient care and improved patient satisfaction when:
- Procedures are completed once because the staff could effectively and efficiently do it correctly the first time
- Appropriate care is provided because errors are not made that might be related to fatigue or limited focus
- Patients are more confident in the services they receive because staff treating them are more positive and energetic when providing care
These are just a few ways that an ergonomic workstation can improve patient care.
Why You Should Work with Double Black Imaging for Your Radiology Workstations
At Double Black Imaging, we don’t just sell you equipment to meet a standard ergonomic need. We complete an onsite radiology workstation survey to assess what ergonomic equipment will be best for you and your radiologists.
We make specific recommendations for each surveyed workspace. Our recommendations for your specific needs are based on our insider knowledge of PACS, mammography/tomography, clinical and surgical applications.
Contact us here, email us, or call us at (877) 852-2870, to arrange your Onsite Radiology Equipment Survey and determine what workstation will be best for you and your radiologists.
References:
- ATD Releases 2016 State of the Industry Report | ATD, January 9, 2023
- Employee Injuries: What Is the Real Cost to Employers? (workplacetesting.com), January 9, 2023
- Prevalence of Musculoskeletal Work-related Injuries Among Radiation Therapists – PubMed (nih.gov), January 9, 2023 Hanania AN, Cook A, Threadgill MP, Conway SH, Ludwig M. Prevalence of Musculoskeletal Work-related Injuries Among Radiation Therapists. Radiol Technol. 2020 May;91(5):414-421. PMID: 32381659.












 Double Black Imaging
Double Black Imaging When it comes to making an important investment in your healthcare facility, you want to make sure you do so through a reliable company that has a thorough understanding of your needs. With over 30 years of experience in the
When it comes to making an important investment in your healthcare facility, you want to make sure you do so through a reliable company that has a thorough understanding of your needs. With over 30 years of experience in the 

 Complexity of medical diagnosis puts the radiologist in a vulnerable position against making mistakes. It is interesting to note that errors made in clinical diagnosis are positively correlated with the errors made in radiological diagnosis. Thus, it is well worth our time to take a closer look at the errors that could be made and how to prevent these discrepancies in radiology. The following are articulations of how mistakes are easily made within the radiology sector.
Complexity of medical diagnosis puts the radiologist in a vulnerable position against making mistakes. It is interesting to note that errors made in clinical diagnosis are positively correlated with the errors made in radiological diagnosis. Thus, it is well worth our time to take a closer look at the errors that could be made and how to prevent these discrepancies in radiology. The following are articulations of how mistakes are easily made within the radiology sector.
 Many people have a tendency to
Many people have a tendency to